
Testing of reflexes.
The peripheral nervous system (PNS) is composed of cranial nerves, spinal nerves, the distal branches of these nerves, and ganglia. Any disorder of nerve function is called a neuropathy. Your textbook describes methods of testing for neuropathies of the cranial nerves. The spinal cord and spinal nerves are tested by assessing various somatic reflexes. Testing a reflex helps a clinician evaluate not only the individual components of a reflex arc (receptors, neurons, and muscles) but also the overall state of the nervous system. Abnormalities of reflex function, coupled with other information gathered during the physical examination, provide valuable clues to diagnosis. One advantage of reflex testing is that it is easy to do; it requires only simple tools and good powers of observation. Although just a few reflexes are routinely tested, many others can be tested if necessary. Reflexes are usually graded on a scale of 0 to 4+:
0 Areflexia, absence of response
1+ Hyporeflexia, a somewhat diminished response
2+ An average or normal response
3+ Hyperreflexia, a stronger than normal response, possibly indicating disease
4+ Intense hyperreflexia with sustained clonus, indicating disease
Areflexia or hyporeflexia typically indicates a segmental lesion of the spinal cord segment or nerve root that innervates the muscle.
Hyperreflexia typically indicates a suprasegmental lesion of higher levels of the CNS that normally inhibit the reflex. The following discussion describes a few of the deep and superficial reflexes most commonly tested in adults and some of the reflexes tested in infants.
Deep Reflexes
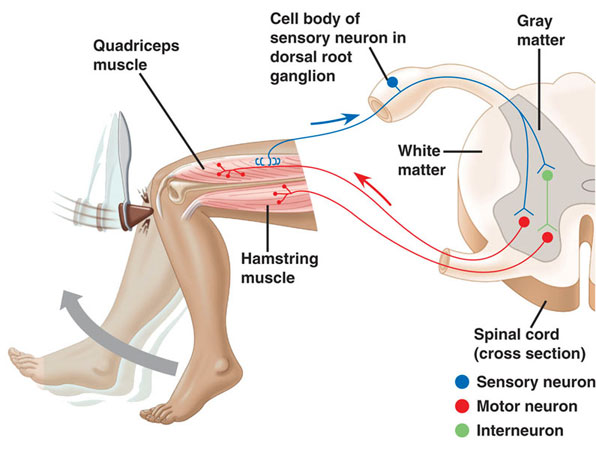
The testing of deep reflexes usually involves striking the skin with a reflex hammer to stretch specific tendons and stimulate the tendon organs and muscle spindles. Clinicians commonly test the biceps, knee, and ankle reflexes and may test for clonus.
Biceps Reflex
The patient lies supine with the elbow flexed about 30°. The clinician presses on the cubital fossa to stretch the biceps tendon and strikes his or her own fingers with the reflex hammer. In a normal response, the biceps should contract slightly, but not enough to flex the elbow. If there is a lesion of the musculocutaneous nerve or segment C6 of the spinal cord, the biceps does not contract but the finger flexors may contract slightly. If there is a suprasegmental lesion, the biceps may contract more forcefully than normal and the brachioradialis or finger flexors may contract.

Knee Reflex
The patient either sits or lies supine with the knee flexed 90°. The examiner strikes the patellar ligament with the reflex hammer. Normal responses range from a slight twitch of the quadriceps femoris muscle t o extension of the knee, lifting the leg. The absence of a response indicates a disease of lumbar nerve roots L3 and L4 or the femoral nerve.
Ankle Reflex
There are several ways to test this reflex. One is to have the patient kneel on the examining table with the foot extending beyond the end of the table. The examiner presses slightly against the foot to dorsiflex it, thus stretching the gastrocnemius muscle, and then strikes the calcaneal tendon with the reflex hammer. The gastrocnemius should contract and plantar flex the foot. Other positions and methods can be tried if this one fails, but if no response is obtained by any method, a disease of the first sacral nerve root or the tibial nerve is indicated.


Clonus
Clonus was described in the preceding chapter in connection with epilepsy (clonic seizures), but it can also be elicited in normal persons by the proper test. The patient should lie supine with the hip and knee flexed at 30° to 45° angles. The examiner then produces a sudden and sustained contraction of the gastrocnemius and soleus muscles by passively dorsiflexing the foot. In normal people, the calf muscles contract, relax, and contract again for about two or three beats. This occurs because the contraction of one muscle stimulates the stretch receptors in the antagonistic muscle. When the antagonist contracts, it stimulates the stretch receptors in the original muscle and triggers a reflex contraction. In people with suprasegmental lesions, the clonus continues for as long as the examiner dorsiflexes the patient’s foot.
Superficial Reflexes
Superficial reflexes are tested by stimulating the skin. Following are three examples of these tests.
Abdominal Reflex
The patient must be supine and relaxed. The examiner strokes the skin of the abdomen with a pointed object such as a pencil or the handle of a reflex hammer, moving from the lateral margins of the abdomen toward the midsagittal plane along a given dermatome. Normally, the underlying muscle contracts and pulls the umbilicus toward the stimulus. An absence of response in a given dermatome may indicate lesions to spinal nerves or roots T7 to T11. The response is often absent, however, in elderly patients and people with lax abdominal muscles.
Cremasteric Reflex
In males, stroking the inner, upper aspect of the thigh with a pin or pencil point causes the ipsilateral testicle (but not the scrotum) to rise, owing to contraction of the cremaster muscle. Lesions in spinal cord segments or nerve roots L1 to L2 or in the corticospinal tracts abolish this reflex.
Plantar Reflex
To test this reflex, the patient must be supine with the lower limbs extended. The examiner strokes the sole of the foot firmly with the handle point of the reflex hammer, progressing from the heel toward the toes. Normal subjects show a flexor plantar response in which they quickly flex the hip and knee, dorsiflex the ankle, and adduct and plantar flex (curl) the toes. An abnormal extensor plantar (Babinski) response is a reliable, early warning sign of corticospinal tract disease; the patient extends and dorsiflexes the great toe and abducts (fans) the other toes. The extensor plantar response also sometimes occurs in persons unconscious from drug or alcohol intoxication.

Reflexes of Infants
Because the nervous system is not completely developed at birth, neurological examination of infants differs somewhat from the techniques used for adults. Normally, a neonatal examination is performed between 36 and 60 hours after birth. In addition to reflexes, the infant’s motor pattern and body posture are observed. A normal infant has flexed limbs, and its head may be turned to one side. The lower limbs may be moving or kicking, and the infant is expected to become more active and to begin crying during the examination. On the other hand, certain responses are considered abnormal. For instance, an infant extending its limbs may have suffered intracranial hemorrhage. Asymmetric behavior of the upper limbs suggests brachial plexus palsy. Lack of increased activity during the examination suggests anoxia or intracerebral hemorrhage. Infants are tested for the same reflexes asadults as well as some additional ones described here.


The trunk incurvation (Galant) reflex is tested by stroking the back from the shoulder to the buttocks or vice versa, about 1 cm from the midline. This stimulus should elicit contraction of the ipsilateral back muscles, causing the infant’s shoulders and pelvis to curve toward the stimulus while the trunk curves away. This response normally disappears at 2 months of age. Its earlier absence may indicate a transverse spinal cord lesion.

The grasp reflex is evaluated by determining the infant’s ability to forcefully grasp the examiner’s hand when the ulnar palmar surface is stimulated. This reflex normally disappears at 3 t o 4 months of age. Persistence of the reflex beyond 4 months may indicate cerebral dysfunction.

The rooting reflex is a response to tactile stimulation of the lips. When the corner of the baby’s mouth is stroked, the baby opens its mouth and turns its head toward that side. When the midline of the upper lip is stroked, the baby extends its head, and when the midline of the lower lip is stroked, the jaw drops. This reflex disappears at 3 to 4 months of age, although sleeping infants exhibit it at slightly older ages. Absence of this reflex before 3 to 4 months indicates severe CNS disease.

The startle (Moro) reflex is a response to a sudden stimulus such as a jolt, a loud noise, or being dropped a short distance (supporting the baby in a supine position and suddenly lowering it about 2 feet). The normal response is for the infant t o extend and abduct all four limbs and extend and fan the digits, then flex and adduct the limbs. Neurologic disease is suspected if this reflex persists beyond 4 months and is almost certain if it persists beyond 6 months. An asymmetric response may indicate hemiparesis, brachial plexus injury, or fracture of the clavicle or humerus. The absence of a startle reflex may indicate kernicterus—damage to the basal nuclei or other areas of the CNS by accumulated bilirubin, a hemoglobin breakdown product seen in hemolytic disease of the newborn and some other conditions.

Irrespective of receiving daily oral or future injectable depot therapies, these require health care visits for medication and monitoring of safety and response. If patients are treated early enough, before a lot of immune system damage has occurred, life expectancy is close to normal, as long as they remain on successful treatment. However, when patients stop therapy, virus rebounds to high levels in most patients, sometimes associated with severe illness because i have gone through this and even an increased risk of death. The aim of “cure”is ongoing but i still do believe my government made millions of ARV drugs instead of finding a cure. for ongoing therapy and monitoring. ARV alone cannot cure HIV as among the cells that are infected are very long-living CD4 memory cells and possibly other cells that act as long-term reservoirs. HIV can hide in these cells without being detected by the body’s immune system. Therefore even when ART completely blocks subsequent rounds of infection of cells, reservoirs that have been infected before therapy initiation persist and from these reservoirs HIV rebounds if therapy is stopped. “Cure” could either mean an eradication cure, which means to completely rid the body of reservoir virus or a functional HIV cure, where HIV may remain in reservoir cells but rebound to high levels is prevented after therapy interruption.Dr Itua Herbal Medicine makes me believes there is a hope for people suffering from,Parkinson's disease,Schizophrenia,Cancer,Scoliosis,Fibromyalgia,Fluoroquinolone Toxicity
ResponderEliminarSyndrome Fibrodysplasia Ossificans Progressiva.Fatal Familial Insomnia Factor V Leiden Mutation ,Epilepsy Dupuytren's disease,Desmoplastic small-round-cell tumor Diabetes ,Coeliac disease,Creutzfeldt–Jakob disease,Cerebral Amyloid Angiopathy, Ataxia,Arthritis,Amyotrophic Lateral Sclerosis,Alzheimer's disease,Adrenocortical carcinoma.Asthma,Allergic diseases.Hiv_ Aids,Herpe ,Copd,Diabetes,Hepatitis,I read about him online how he cure Tasha and Tara so i contacted him on drituaherbalcenter@gmail.com even talked on whatsapps +2348149277967 believe me it was easy i drank his herbal medicine for two weeks and i was cured just like that isn't Dr Itua a wonder man? Yes he is! I thank him so much so i will advise if you are suffering from one of those diseases Pls do contact him he's a nice man.