Muscular System

The muscular system is an organ system consisting of skeletal, smooth and cardiac muscles. It permits movement of the body, maintains posture, and circulates blood throughout the body. The muscular system in vertebrates is controlled through the nervous system, although some muscles (such as the cardiac muscle) can be completely autonomous.
Muscles.
There are three distinct types of muscles: skeletal muscles, cardiac or heart muscles, and smooth (non-striated) muscles. Muscles provide strength, balance, posture, movement and heat for the body to keep warm.
Upon stimulation by an action potential, skeletal muscles perform a coordinated contraction by shortening each sarcomere. The best proposed model for understanding contraction is the sliding filament model of muscle contraction. Actin and myosin fibers overlap in a contractile motion towards each other. Myosin filaments have club-shaped heads that project toward the actin filaments.
Larger structures along the myosin filament called myosin heads are used to provide attachment points on binding sites for the actin filaments. The myosin heads move in a coordinated style, they swivel toward the center of the sarcomere, detach and then reattach to the nearest active site of the actin filament. This is called a rachet type drive system. This process consumes large amounts of adenosine triphosphate (ATP).
Energy for this comes from ATP, the energy source of the cell. ATP binds to the cross bridges between myosin heads and actin filaments. The release of energy powers the swiveling of the myosin head. Muscles store little ATP and so must continuously recycle the discharged adenosine diphosphate molecule (ADP) into ATP rapidly. Muscle tissue also contains a stored supply of a fast acting recharge chemical, creatine phosphatewhich can assist initially producing the rapid regeneration of ADP into ATP.
Calcium ions are required for each cycle of the sarcomere. Calcium is released from the sarcoplasmic reticulum into the sarcomere when a muscle is stimulated to contract. This calcium uncovers the actin binding sites. When the muscle no longer needs to contract, the calcium ions are pumped from the sarcomere and back into storage in the sarcoplasmic reticulum.
Muscular atrophies.
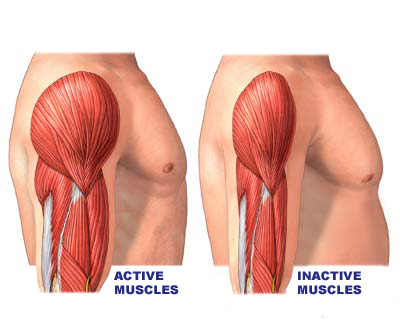
Muscle atrophy, or disuse atrophy, is defined as a decrease in the mass of the muscle; it can be a partial or complete wasting away of muscle. When a muscle atrophies, this leads to muscle weakness, since the ability to exert force is related to mass. Muscle atrophy results from a co-morbidity of several common diseases, including cancer, AIDS, congestive heart failure, COPD (chronic obstructive pulmonary disease), renal failure, and severe burns; patients who have "cachexia" in these disease settings have a poor prognosis. Moreover, starvation eventually leads to muscle atrophy. Disuse of the muscles will also lead to atrophy.
Botulism
What is botulism?
Botulism is a rare but serious paralytic illness caused by a nerve toxin that is produced by the bacterium Clostridium botulinum and sometimes by strains of Clostridium butyricum and Clostridium baratii. There are five main kinds of botulism. Foodborne botulism is caused by eating foods that contain the botulinum toxin. Wound botulism is caused by toxin produced from a wound infected with Clostridium botulinum. Infant botulism is caused by consuming the spores of the botulinum bacteria, which then grow in the intestines and release toxin. Adult intestinal toxemia (adult intestinal colonization) botulism is a very rare kind of botulism that occurs among adults by the same route as infant botulism. Lastly, iatrogenic botulism can occur from accidental overdose of botulinum toxin. All forms of botulism can be fatal and are considered medical emergencies. Foodborne botulism is a public health emergency because many people can be poisoned by eating a contaminated food.
What kind of germ is Clostridium botulinum?
Clostridium botulinum is the name of a group of bacteria. They can be found in soil. These rod-shaped organisms grow best in low oxygen conditions. The bacteria form spores which allow them to survive in a dormant state until exposed to conditions that can support their growth. There are seven types of botulism toxin designated by the letters A through G; only types A, B, E and F cause illness in humans.
What are the symptoms of botulism?
The classic symptoms of botulism include double vision, blurred vision, drooping eyelids, slurred speech, difficulty swallowing, dry mouth, and muscle weakness. Infants with botulism appear lethargic, feed poorly, are constipated, and have a weak cry and poor muscle tone. These are all symptoms of the muscle paralysis caused by the bacterial toxin. If untreated, these symptoms may progress to cause paralysis of the respiratory muscles, arms, legs, and trunk. In foodborne botulism, symptoms generally begin 18 to 36 hours after eating a contaminated food, but they can occur as early as 6 hours or as late as 10 days.
How is botulism diagnosed?
Physicians may consider the diagnosis if the patient's history and physical examination suggest botulism. However, these clues are usually not enough to allow a diagnosis of botulism. Other diseases such as Guillain-Barré syndrome, stroke, and myasthenia gravis can appear similar to botulism, and special tests may be needed to exclude these other conditions. These tests may include a brain scan, spinal fluid examination, nerve conduction test (electromyography, or EMG), and a tensilon test for myasthenia gravis. Tests for botulinum toxin and for bacteria that cause botulism can be performed at some state health department laboratories and at CDC.
How can botulism be treated?
The respiratory failure and paralysis that occur with severe botulism may require a patient to be on a breathing machine (ventilator) for weeks or months, plus intensive medical and nursing care. The paralysis slowly improves. Botulism can be treated with an antitoxin which blocks the action of toxin circulating in the blood. Antitoxin for infants is available from the California Department of Public Health, and antitoxin for older children and adults is available through CDC.If given before paralysis is complete, antitoxin can prevent worsening and shorten recovery time. Physicians may try to remove contaminated food still in the gut by inducing vomiting or by using enemas. Wounds should be treated, usually surgically, to remove the source of the toxin-producing bacteria followed by administration of appropriate antibiotics. Good supportive care in a hospital is the mainstay of therapy for all forms of botulism.
Tetanus
etanus is an infectious disease caused by contamination of wounds from the bacteria Clostridium tetani, or the spores they produce that live in the soil, and animal feces. Tetanus has been recognized for centuries; the term is derived from the ancient Greek wordstetanos and teinein, meaning taut and stretched, which describe the condition of the muscles affected by the toxin, tetanospasm, produced by Clostridium tetani. The causative bacterium,Clostridium tetani, is a hardy organism capable of living many years in the soil in a form called a spore. The bacterium was first isolated in 1889 by S. Kitasato while he was working with R. Koch in Germany. Kitasato also found the toxin responsible for tetanus and developed the first protective vaccine against the disease.
Tetanus occurs when a wound becomes contaminated with Clostridium tetanibacterial spores. Infection follows when spores become activated and develop into gram-positive bacteria that multiply and produce a very powerful toxin (tetanospasmin) that affects the muscles. Tetanus spores are found throughout the environment, usually in soil, dust, and animal waste. The usual locations for the bacteria to enter the body are puncture wounds, such as those caused by rusty nails, splinters, or insect bites. Burns, any break in the skin, and IV drug access sites are also potential entryways for the bacteria. Tetanus is acquired through contact with the environment; it is not transmitted from person to person.
Tetanus results in severe, uncontrollable muscle spasms. For example, the jaw is "locked" by muscle spasms, causing the disease to sometimes be called "lockjaw." In severe cases, the muscles used to breathe can spasm, causing a lack of oxygen to the brain and other organs that may possibly lead to death.
- The disease can show four possible types:
- Generalized tetanus can affect all skeletal muscles. It is the most common as well as the most severe form of the four types.
- Local tetanus manifests with muscle spasms at or near the wound that has been infected with the bacteria.
- Cephalic tetanus primarily affects one or several muscles in the face rapidly (in one to two days) after a head injury or ear infection. Trismus ("lockjaw") may occur. The disease can easily progress to generalized tetanus.
- Neonatal tetanus is similar to generalized tetanus except that it affects a baby that is less than 1 month old (called a neonate). This condition is rare in developed countries.
Tetanus Causes
Clostridium tetani is a gram-positive rod-shaped bacterium that is found worldwide in soil; it is usually in its dormant form, spores, and becomes the rod-shaped bacterium when it multiplies. The vegetative rods produce the spore usually at one end of the rod. The organisms are considered anaerobic.
- Clostridium tetani is the bacterium responsible for the disease. The bacteria are found in two forms: as a spore (dormant) or as a vegetative cell (active) that can multiply.
- The spores are in soil, dust, and animal waste and can survive there for many years. These spores are resistant to extremes of temperature.
- Contamination of a wound with tetanus spores is rather common. Tetanus, however, can only occur when the spores germinate and become active bacterial cells.
- The active bacterial cells release two exotoxins, tetanolysin and tetanospasmin. The function of tetanolysin is unclear, but tetanospasmin is responsible for the disease.
- The disease typically follows an acute injury or trauma that results in a break in the skin. Most cases result from a puncture wound, laceration (cut), or an abrasion (scrape).
- Other tetanus-prone injuries include the following:
- frostbite,
- surgery,
- crush wound,
- abscesses,
- childbirth,
- IV drug users (site of needle injection).
- Wounds with devitalized (dead) tissue (for example, burns or crush injuries) or foreign bodies (debris in them) are most at risk of developing tetanus.
- Tetanus may develop in people who are not immunized against it or in people who have failed to maintain adequate immunity with active booster doses of vaccine.

The hallmark feature of tetanus is muscle rigidity and spasms.
- In generalized tetanus, the initial complaints may include any of the following:
- Irritability, muscle cramps, sore muscles, weakness, or difficulty swallowing are commonly seen.
- Facial muscles are often affected first.Trismus or lockjaw is most common. This condition results from spasms of the jaw muscles that are responsible for chewing. A sardonic
smile -- medically termed risussardonicus -- is a characteristic feature that results from facial muscle spasms. - Muscle spasms are progressive and may include a characteristic arching of the back known as opisthotonus. Muscle spasms may be intense enough to cause bones to break and joints to dislocate.
- Severe cases can involve spasms of the vocal cords or muscles involved in breathing. If this happens, death is likely, unless medical help (mechanical ventilation with a respirator) is readily available.
 |
| Picture of opisthotonus or arched back due to muscle spasms in a person with generalized tetanus |
- In cephalic tetanus, in addition to lockjaw, weakness of at least one other facial muscle occurs. In two-thirds of these cases, generalized tetanus will develop.
- In localized tetanus, muscle spasms occur at or near the site of the injury. This condition can progress to generalized tetanus.
- Neonatal tetanus is identical to generalized tetanus except that it affects the newborn infant. Neonates may be irritable and have poor sucking ability or difficulty swallowing.
Tetanus Diagnosis
The diagnosis of generalized tetanus is usually made by observing the clinical presentation and a combination of the following:
- History of a recent injury resulting in skin breakage (but this is not universal; only 70% of cases have an identified injury)
- Incomplete tetanus immunizations
- Progressive muscle spasms (starting in the facial region, especially lockjaw and progressing outward from the face to include all muscles of the body)
- Fever
- Changes in blood pressure (especially high blood pressure)
- Irregular heartbeat
- In localized tetanus, pain, cramps, or muscle spasms occur at or near a recent skin injury.
- Neonates show signs of being generally irritable, muscle spasms, and poor ability to take in liquids (poor sucking response), usually seen in neonates about 7-10 days old.
- Laboratory tests are rarely used to diagnose tetanus. However, some reference labs can determine if the patient has serum antitoxin levels that are protective, and thus a positive test detecting these levels suggests that the diagnosis of tetanus is unlikely.
Medical Treatment for Tetanus
Medical treatment has two aims: limit growth and eventually kill the infecting C. tetani and thus eliminate toxin production; the second aim is to neutralize any toxin that is formed. If the toxin has already affected the patient, the two aims are still important, but supportive measures will be needed for the patient. These steps are outlined below:
- Antibiotics (for example, metronidazole[Flagyl, Flagyl 375, Flagyl ER], penicillin G or doxycycline [Adoxa, Alodox, Avidoxy, Doryx, Monodox, Oracea, Oraxyl, Periostat, Vibramycin, Vibramycin Calcium, Vibramycin Monohydrate, Vibra-Tabs]) to kill the bacteria, tetanus booster shot, if necessary, and occasionally, antitoxin (termed tetanus immune globulin or TIG) to neutralize the toxin
- Wound cleansing to remove any obvious bacteria collections (abscesses) or foreign bodies; if the patient is exhibiting any toxin-related problems, TIG is usually administered first and wound care is delayed for a few hours while the TIG neutralizes toxin because infected wounds, when manipulated, may release more toxin
- Supportive measures
- Pain medicine as needed
- Sedatives such as diazepam (Valium) to control muscle spasms and muscle relaxants
- Ventilator support to help with breathing in the event of spasms of the vocal cords or the respiratory muscles
- IV rehydration because, as muscles spasm constantly, increased metabolic demands are placed on the body
No hay comentarios:
Publicar un comentario